The respiratory system’s basic defense mechanism, coughing, often goes undetected until it becomes chronic and persistent. This chronic cough may be a sign of underlying problems, and the complex relationship between allergens and cough has received more attention recently. In this extensive investigation, we take a deep dive into the intricate connection and discover the intricacies of how allergens may cause and aggravate cough. We will explore the many allergy types that are involved, the underlying physiological mechanisms that are at work, and the various treatment options that work.
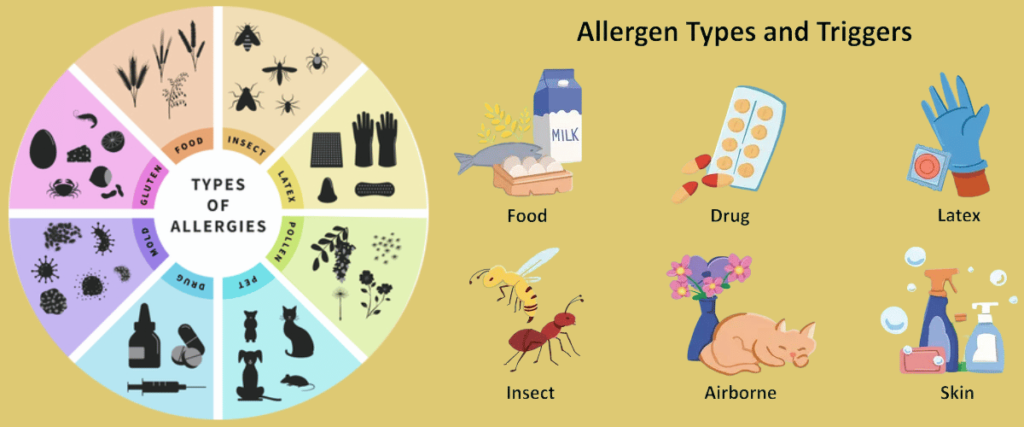
Knowing About Allergies
Coughing is just one of the many ways that an allergy may present itself. One type of cough is called an allergy-triggered cough, cough-variant asthma, or allergic rhinitis. The following lists and categorizes allergies that cause coughing:
1. Hay fever, or allergic rhinitis
- An inflammatory reaction to airborne allergens, mainly dust mites, mold spores, pet dander, or pollens, is known as allergic rhinitis.
- Cough Connection: Postnasal drip frequently causes a dry, persistent cough in people with allergic rhinitis. This happens when the back of the throat becomes irritated by mucus produced in reaction to allergens.
2. Allergies to the Environment
- Allergies brought on by external elements like pollen, dust mites, mold, and air pollution.
- Relationship to Coughing: Being around these allergens may irritate the respiratory tract and increase mucus production, both of which can result in a persistent cough.
3. Allergies to pet dander
- Cats’ skin cells, saliva, and urine contain proteins that can cause allergic reactions.
- Connection to Coughing: Breathing in pet dander can irritate the respiratory tract, which can result in coughing, particularly in those who are more sensitive.
4. Allergies to mold
- Allergies to mold spores in the air that are frequently present in moist environments.
- Connection to Coughing: Breathing in mold spores can set off an immunological reaction that results in respiratory symptoms, such as coughing.
5. Asthma Allergic
- Allergies aggravate asthma by narrowing the airways and causing inflammation in the asthmatic.
- Relation to Coughing: When wheezing is absent, coughing is a common symptom of allergic asthma.
6. Allergies to Food
- An allergic response to particular foods, such as dairy, shellfish, or nuts.
- Connection to Coughing: Because food allergies release histamine and other inflammatory mediators, they can occasionally cause respiratory symptoms like coughing.
7. Allergies at Work
- The term describes allergies brought on by being around allergens such dust, chemicals, or fumes at work.
- Connection Between Coughing and Occupational Allergens: In people who are sensitive, occupational allergens can aggravate the airways and cause coughing.
8. Allergies to Smoke and Air Pollution
- Airborne pollutants or smoke can cause sensitivity.
- The Connection Between Smoke and Coughing: Inhaling smoke or other air pollutants can irritate respiratory tracts in people who are allergic to them, leading to coughing.
9. Respiratory infections and allergies
- Allergies may make a person more susceptible to respiratory infections.
- Connection to Coughing: Because allergies stimulate the immune system, they can make respiratory infections worse when it comes to coughing.
10. Gastroesophageal reflux disease (GERD) and allergies
- Gerd, or reflux of stomach acid into the esophagus, is the cause of symptoms that resemble heartburn.
- The Connection Between Coughing and Acid Reflux Disease (GERD): Asthma reactions can aggravate coughing because they irritate the esophagus.
The phenomenon of allergic cough is complex and influenced by different allergens and immune responses. For the cough to be effectively managed, it is essential to determine which allergen is causing it. Allergy relief and improved respiratory health can be achieved by consulting a physician, getting tested for allergies, and using the right treatment plans.
How Allergy Reactions Work
Allergy reactions are intricate reactions of the immune system to normally harmless substances that are viewed as dangers. Allergens that people can eat, breathe or touch. The allergy in a patient with an active immunity produces certain antibodies that result in a chain reaction in the body systems, leading to allergy symptoms.This is a thorough explanation of how allergic reactions function:
1. Inflammation:
An allergen’s initial exposure frequently causes sensitization. In response to this first encounter, the immune system produces immunoglobulin E (IgE), a particular class of antibody that it recognizes as foreign.
2. Basophil and mast cell activation:
IgE antibodies bind to mast cells and basophils, which are specialized cells present in different body tissues and are particularly abundant in areas that are susceptible to allergen exposure (e.g., skin, lungs, digestive system).
3. Following Exposure:
The allergen attaches itself to the IgE antibodies on the surface of basophils and mast cells after being exposed to it again.
4. Inflammatory mediators are released:
Histamine is one of the inflammatory mediators that are released from mast cells and basophils when an allergen binds to IgE.
5. Reaction to Inflammation:
Blood vessel dilatation, increased blood vessel wall permeability, and nerve end stimulation are all brought on by histamine and other mediators. This causes the typical allergic reaction symptoms, which include increased mucus production, redness, swelling, and itching.
6. Typical Sensitive Symptoms:
The particular allergen and exposure route determine the symptoms. Typical signs of allergies include:
- Sneezing, coughing, wheezing, dyspnea, and nasal congestion are examples of respiratory symptoms.
- Symptoms of the skin: redness, swelling, hives, itching.
- Symptoms of the digestive system: vomiting, diarrhea, nausea, and abdominal pain.
- Systemic Symptoms: Malaise, exhaustion, and fever (in cases of severe reactions).
7. Late-Stage Response:
A late-phase reaction can sometimes happen hours or even days after the initial exposure. Persistent symptoms are indicative of this prolonged response, which may also entail the recruitment of additional immune cells.
8. Anaphylaxis
A severe allergic reaction with a high potential for death is anaphylaxis. It involves a systemic response brought on by the widespread release of inflammatory mediators. Breathing difficulties, a decrease in blood pressure, and unconsciousness are signs of anaphylaxis.
9. Allergic Chronic Conditions:
Chronic allergic illnesses that can arise from recurrent exposure to allergens include allergic rhinitis, asthma, and atopic dermatitis. The immune systems of these diseases are hyperresponsive and exhibit chronic inflammation.
10. Recognition and Handling:
Allergists use a variety of methods, such as skin prick and blood tests, to identify allergies. Avoiding allergens, taking medicine (corticosteroids, antihistamines, etc.), and allergen-specific immunotherapy (desensitization) are a few of the potential treatment options.
Effective allergy management requires an understanding of the processes behind allergic responses. Many allergic responses are not serious, but others can be and need to be treated by a doctor right once. People who are aware of their allergies should collaborate closely with medical specialists to create individualized treatment plans and be ready for any emergency, particularly in the event of severe allergic responses such as anaphylaxis.
The Cough Response and the Respiratory System:
A. Respiratory System Anatomy
A review of the architecture of the respiratory system is necessary to comprehend how allergens might affect cough. To enable gas exchange and preserve airway health, the upper and lower respiratory tracts—which include the lungs and bronchial tree—cooperate.
B. The Reflex Cough
The purpose of the complex neurological network that is the cough reflex, which includes the brainstem, vagus nerve, and other receptors, is to rid the airways of irritating substances. This reflexive activity emphasizes the significance of maintaining adequate lung function by precisely regulating the respiratory system.
Cough and Allergies: The Complicated Relationship
A. Typical Allergens Causing Cough
Some allergens are particularly well-known for causing cough symptoms. Allergy triggers that are seasonal (pollen, grass, and mold spores) and perennial (dust mites, pet dander, and cockroach droppings) are well-known causes of allergic cough.
B. The Mechanisms of Cough Induced by Allergies
There is a series of steps involved in the process from allergen exposure to cough manifestation. The scene is set by an inflammatory response in the airways that is typified by increased mucus production and airway hyperreactivity. Concomitantly, the activation of sensory nerves triggers the cough reflex, which leads to the typical cough observed in allergy-related situations.
Medicinal Display
A. Symptoms of Allergic Cough
The symptoms of an allergic cough are unique, so it’s important to recognize them. Usually, this type of cough is dry and persistent, and it can come with other classic allergy symptoms like sneezing, stuffy nose, and watery eyes, which together create a constellation of allergic manifestations.
B. Diagnosis Differential
The difficult part is telling an allergic cough apart from other respiratory ailments. This calls for a thorough process that includes a thorough physical examination, a detailed medical history, and the prudent use of diagnostic tests to rule out other possible diagnoses.
Diagnosis
A. Medical Assessment
The process of diagnosing entails a number of steps, starting with allergy testing techniques like blood or skin prick tests to pinpoint particular allergens. Furthermore, pulmonary function tests are essential for evaluating the responsiveness and function of the airways.
B. Imaging’s Function
Imaging modalities such as CT scans and chest X-rays are invaluable in ruling out structural abnormalities and giving a more comprehensive picture of the respiratory landscape, even though they may not be able to directly identify allergic causes.
Therapy and Administration
A. Avoiding Allergens
The key to treating allergic cough is minimizing exposure to allergens. Techniques include everything from practical changes in the home and office to environmental ones like using air purifiers.
B. Pharmacological Interventions
| Medication Class | Examples | Mechanism of Action | Considerations |
|---|---|---|---|
| Antihistamines | Loratadine (Claritin), Cetirizine (Zyrtec) | Block histamine receptors, reducing allergic symptoms | May cause drowsiness; choose non-sedating formulations |
| Decongestants | Pseudoephedrine, Phenylephrine | Constrict blood vessels, reducing nasal congestion | Short-term use; caution in individuals with hypertension |
| Corticosteroids | Fluticasone (Flonase), Budesonide (Rhinocort) | Suppress inflammation, reducing airway hyperreactivity | Considered for persistent symptoms; local or systemic use |
| Bronchodilators | Albuterol (Ventolin), Formoterol (Foradil) | Dilate airways, facilitating airflow and relieving cough | Use as needed for acute symptom relief |
C. Immunotherapy
Allergen-specific immunotherapy, also referred to as allergy shots, is a potentially effective long-term solution. In order to lessen allergic reactions and desensitize the immune system, this entails exposing people to allergens gradually.
Modifications to Lifestyle
A. Controls for the environment
A home can be made allergy-free by carefully using air purifiers, getting enough ventilation, and keeping humidity levels at ideal levels. All of these actions combined make living conditions for allergy sufferers more comfortable.
B. Nutritional Factors
A developing area of allergy management is investigating dietary changes. Although specific foods may affect allergic reactions, following an allergy-friendly diet may enhance conventional treatment methods.
Long-Term Prospects and Difficulties
A. The Allergic Cough’s Chronicity
It is crucial to comprehend the elements influencing the symptoms’ persistence in order to develop long-term treatment plans. Making lifestyle changes, adhering to treatment plans consistently, and scheduling routine follow-ups all help to improve the prognosis for people suffering from allergy-induced cough.
B. Difficulties
Apart from the somatic manifestations, an allergic cough can result in extensive ramifications. It affects life quality as well as having the potential to cause the onset or worsening of diseases like asthma. Identifying and managing these issues are essential components of a comprehensive approach to healthcare.
Conclusion
We have examined a range of factors in an attempt to determine how allergens and chronic cough are related, including hay fever and environmental irritants. Understanding the immune response, from sensitization to inflammatory mediators, provides the foundation for effective therapy. Immunotherapy and avoiding allergens are two treatment methods that give promise.
For long-lasting relief, realizing the significance of lifestyle changes—from food modifications to environmental controls—becomes essential. Given that allergic cough is persistent, treatment regimens must be consistently followed. Notwithstanding the intricacies, our investigation underscores the proactive function of healthcare in augmenting respiratory health and general well-being.
Sources:
- https://newsinhealth.nih.gov/2014/10/cold-flu-or-allergy
- https://www.ncbi.nlm.nih.gov/books/NBK447112/
How do you know if your cough is from allergies?
It is important to evaluate associated symptoms like sneezing, itchy eyes, and a runny nose in order to determine whether your cough is due to allergies. A chronic, dry cough that gets worse in certain situations or seasons is probably allergic in nature. Seeking the guidance of a healthcare expert for accurate diagnosis and allergy testing can offer clarity and direct the most suitable course of therapy.
How do you stop an allergy cough?
Use antihistamines to lessen symptoms, think about using nasal corticosteroids for inflammation, decrease exposure to allergens, and seek tailored guidance and treatment from a healthcare provider to relieve an allergy cough.
What does an allergy cough sound like?
Unlike the productive, moist noises that are frequently associated with coughs due to respiratory illnesses, an allergy cough usually sounds dry and persistent.
How long does an allergy cough last?
An allergy cough can linger for weeks or months, depending on the allergen and how long the patient is exposed to it. The length and intensity of the cough can be decreased by controlling allergen exposure and obtaining the right care. Seeking advice and additional assessment from a healthcare provider is recommended if the cough doesn’t go away.
How do I get rid of allergy cough naturally?
To relieve allergy cough naturally:
• Prevent Allergens: Recognize them and reduce your exposure.
• Maintain Hydration: Sip a lot of water.
• Honey: Take advantage of honey’s calming effects.
• Breathe in steam to relieve discomfort.
• Gargle with saltwater to soothe your throat.
• Foods High in Quercetin: These include onions, berries, and apples.
• Probiotics: Use food or supplements to support gut health.



3 thoughts on “Can Allergies Cause a Cough? Symptoms, Signs, and Causes”